Introduction: Understanding Sciatica Surgery
Is sciatica surgery dangerous? If you’re suffering from sciatica, this is likely a question that has crossed your mind. The pain can be debilitating—radiating from your lower back down to your leg, making even simple tasks a struggle. While surgery can provide long-term relief, it’s essential to weigh the benefits and potential risks before making such a significant decision. This guide will help you explore whether sciatica surgery is the right option for you, what the risks are, and how it can improve your quality of life.
You want to also look at this: Hope for Sciatic Nerve and Hip Pain Sufferers: Proven Steps to Regain Comfort and Mobility
What is Sciatica and When Does Surgery Become an Option?
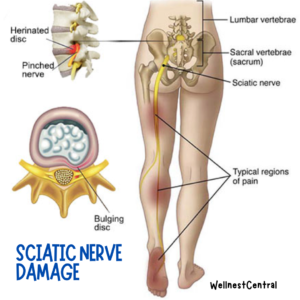
Sciatica is a condition characterized by pain radiating along the sciatic nerve, which branches from your lower back through your hips, buttocks, and down each leg. Common causes of sciatica include:
- Herniated or slipped disc: A disc presses on the sciatic nerve.
- Spinal stenosis: Narrowing of the spinal canal puts pressure on the nerve.
- Degenerative disc disease: Discs between the spine wear down over time.
- Bone spurs or spinal tumors: Abnormal growths that compress the sciatic nerve.
Symptoms of sciatica vary but typically include sharp or burning pain, numbness, tingling, and muscle weakness. Sciatica often improves with conservative treatments such as physical therapy, anti-inflammatory medications, heat/cold therapy, and lifestyle modifications like stretching and exercise.
However, sciatica surgery is usually recommended when:
- Pain is severe and unrelenting despite non-surgical treatments.
- There is significant weakness or loss of bowel/bladder control.
- The condition severely impacts mobility and quality of life.
Different Types of Sciatica Surgery and Their Purposes
There isn’t a one-size-fits-all surgery for sciatica; instead, the type of surgery depends on the cause and severity of the nerve compression. Here are the most common surgical procedures:
- Microdiscectomy:
- A minimally invasive procedure that removes part of a herniated disc pressing on the sciatic nerve.
- Often used for people with a slipped or ruptured disc.
- Laminectomy (also called decompression surgery):
- Involves removing a part of the vertebrae, known as the lamina, to relieve pressure on the sciatic nerve.
- Typically recommended for those with spinal stenosis or tumors causing compression.
- Spinal Fusion:
- The joining of two or more vertebrae to stabilize the spine.
- Generally performed when there’s spinal instability, severe disc degeneration, or other structural problems.
These procedures aim to relieve the pressure on the sciatic nerve, thus reducing pain and improving mobility.
Understanding the Risks: Is Sciatica Surgery Dangerous?
Like any surgery, sciatica surgery does carry some risks. However, the danger varies depending on the individual, the type of surgery, and the surgeon’s experience. Here are some potential risks:
- General Surgical Risks:
- Infection: Like any surgical procedure, there is a risk of infection at the incision site or around the spine.
- Bleeding: Excessive bleeding, though rare, can occur during surgery.
- Blood Clots: There’s a small chance of blood clots forming in the legs, which could travel to the lungs (pulmonary embolism).
- Risks Specific to Sciatica Surgery:
- Nerve Damage: Since surgery is performed close to the sciatic nerve, there is a risk of damaging it or nearby nerves, which may lead to numbness, tingling, or persistent pain.
- Spinal Fluid Leak: A tear in the protective covering around the spinal cord may occur, leading to a cerebrospinal fluid leak, which can be managed with additional care or minor corrective surgery.
- Recurrence of Sciatica: In some cases, symptoms may return months or years after surgery, especially if there is further disc degeneration or spinal issues.
- Surgical Risks Based on Procedure Type:
- Microdiscectomy: While minimally invasive and generally successful, a risk of disc re-herniation exists.
- Laminectomy: Can lead to spinal instability in some cases, requiring further treatment or fusion.
- Spinal Fusion: Has a longer recovery period and, in some cases, the fused bones may not heal as expected.
However, it is worth noting that severe complications are rare, and most patients who undergo sciatica surgery experience some relief from their symptoms.
Benefits of Sciatica Surgery: Relief, Recovery, and Improved Quality of Life
For many people, the benefits of surgery far outweigh the risks. If you are a suitable candidate, sciatica surgery can lead to:
- Pain Relief: Significant reduction or complete relief of leg and back pain.
- Improved Mobility: Easier movement and reduced stiffness allow for a return to daily activities and even exercise.
- Quick Recovery: Minimally invasive surgeries like microdiscectomy often allow patients to resume normal activities within weeks.
- High Success Rates: Sciatica surgery, especially for well-selected candidates, has a success rate ranging from 70-90% in terms of pain relief and improved function.
The key to a successful outcome is choosing the right surgery for your condition and ensuring it’s performed by an experienced spinal surgeon.
Preparing for Sciatica Surgery: Tips for a Safe and Successful Outcome
If you’re considering surgery, preparing both mentally and physically can help ensure the best results. Here are some tips:
- Optimize Health Before Surgery: Stop smoking, maintain a healthy weight, and manage any chronic conditions like diabetes or high blood pressure to improve surgical outcomes.
- Preoperative Physical Therapy: Some patients benefit from “prehab,” exercises that strengthen the muscles supporting the spine to speed up recovery.
- Plan for Post-Surgery Care: Arrange for help at home, as you may need assistance with daily activities during the initial recovery period.
- Follow Post-Surgery Instructions: Adhere to your surgeon’s advice on managing pain, gradually resuming physical activity, and any necessary follow-up appointments.
Conclusion: Making the Best Decision for Your Sciatica Treatment
Surgery for sciatica is not inherently dangerous, but it does come with potential risks like any surgical procedure. It has the potential to provide significant relief from pain and improve your overall quality of life. However, the decision should not be taken lightly. Discuss all available treatment options, understand the risks and benefits, and seek guidance from your healthcare provider to choose the path that is best suited for your situation.
Your road to recovery starts with making the right choice for your body and health. Take the time to learn, ask questions, and choose the option that will help you regain your life.
Call to Action
Have you been struggling with sciatica pain and wondering if surgery is the right choice for you? Share your thoughts and questions in the comments below, and let’s support each other in finding the best path to relief!
FAQs
Q: Can sciatica pain come back after surgery?
A: Yes, sciatica symptoms can recur after surgery, especially if there’s additional disc degeneration or new issues in the spine. However, recurrence is less likely when proper post-surgery care and preventive measures are taken.
Q: How long is the recovery period after sciatica surgery?
A: Recovery time varies but generally takes about 4 to 6 weeks for minimally invasive surgeries. Full recovery from procedures like spinal fusion may take longer, often around 3 to 6 months.
Q: Are there non-surgical alternatives that can provide relief?
A: Absolutely! Physical therapy, medications, spinal injections, and lifestyle modifications are often effective in relieving sciatica pain. Surgery is typically the last resort
Introduction to a Related Topic:
Hope for Sciatic Nerve and Hip Pain Sufferers: Proven Steps to Regain Comfort and Mobility
Cardio vs. Strength Training: Finding the Right Balance for Effective Weight Loss